Knee joint arthrosis is a chronic (long) degenerative disease that causes cartilage destruction in the joints.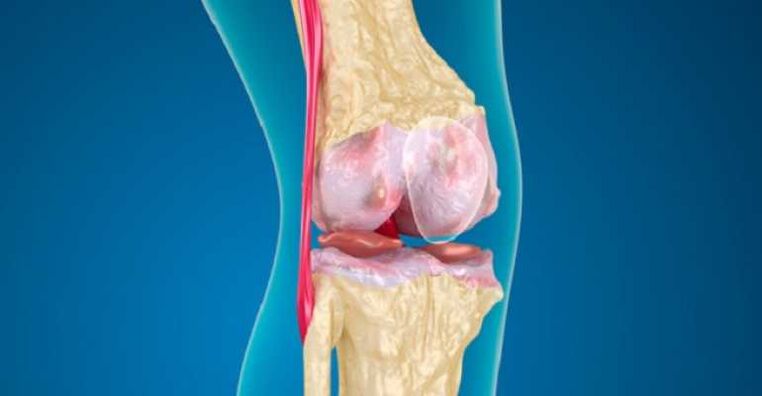 Symptoms include pain, stiffness and swelling.Pain and disability reduction options include lifestyle changes (diet, physical exercise), physical and professional treatment, medication and surgery.
Symptoms include pain, stiffness and swelling.Pain and disability reduction options include lifestyle changes (diet, physical exercise), physical and professional treatment, medication and surgery.
Osteoarthritis of the knee joint
Knee joint osteoarthritis is a conventional disease accompanied by chronic, exhaustive pain.Recent clinical data have shown that central sensitization stimulates osteoarthritis of the knee joint deformity.Improved understanding of how arthrosis of knee joints affects central pain processing is important for identifying new analgesic goals/new therapeutic strategies.
Inhibitory cannabinoid receptors weaken the function of peripheral immune cells and provide central neuro-immune responses to neurogenetic models.The systemic introduction of the receptor agonist has weakened the behavior of the OA, and in this model, changes in circulating pro- and anti-inflammatory cytokines have been identified in this model.
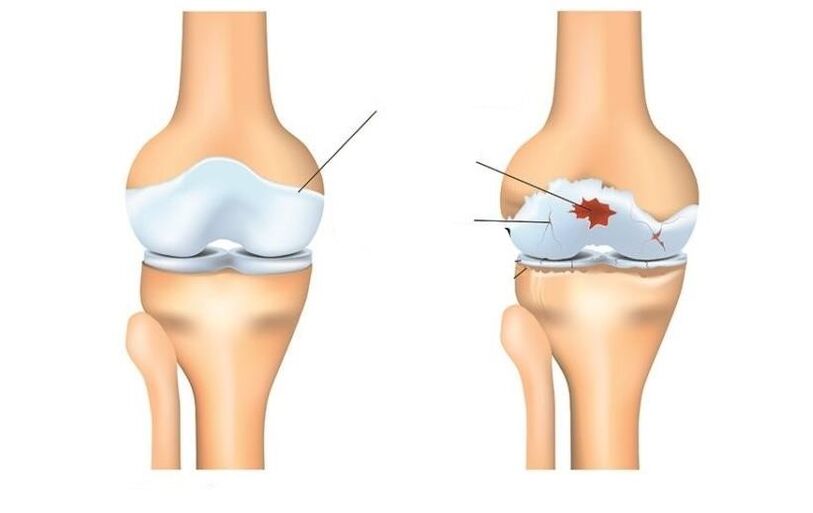
Deformation of arthrosis
Deformed arthrosis of the knee joint is inflammation of the cartilage on the bones and wearing the knee joint (osteo = bone, arthritis = joint, itis = inflammation).The diagnosis of knee joint osteoarthritis is based on two main results: radiographic data on bone health changes (using medical images, such as X-ray and magnetic resonance imaging MRI) and human symptoms.About 14 million people have knee arthrosis.Although it is more common in the elderly, from 14 million to 2 million, who have a knee -related OA, were at the age of 45 and over half older.
Osteoarthritis (OA's knee) is a processing disease caused by inflammation and degeneration of the knee joint that will eventually deteriorate.
It affects the entire joint, including bones, cartilage, ligaments and muscles.Its progression is influenced by age, body mass index (BMI), bone structure, geneticist, muscle strength and activity level.OA knee can also develop as a secondary condition after knee injury.Depending on the stage of the disease and the presence of injuries or conditions, the OA article can be monitored using physical therapy.In more severe or enlarged cases, surgical intervention may be necessary.
Symptoms
Persons who develop knee OA may experience a wide range of symptoms and restrictions on the basis of the progression of the disease.Pain occurs when the cartilage, which includes the knee joint bones, is wearing.The places where the cartilage is rising or damaged will be revealed under the bone.Bone effect allows you to increase stress and cartilage, sometimes even bone contact during movement, which can cause pain.Since the knee is the joint, the level of activity, the level of activity, as well as the type and duration of action, it usually directly affects the symptoms.Symptoms can worsen by weight activity, for example, while walking with a heavy object.
Symptoms of knee joint may include:
- Pain worsening during or after surgery, especially when walking, climbing, downstairs, or moving to sitting.
- Pain or firmness for a long period of bent or straight knee sitting.Pain is the most common symptom of osteoarthritis.As the disease progresses and inflammation progresses, the pain can become permanent.
- Feeling jumping, cracking or grinding when moving the knee.
- Swelling after action.
- The firmness of the affected joint was often found first in the morning and after rest.
- Swelling, which is sometimes warm, can be noticeable in the arthritis joint.
- Deformation can occur due to osteoarthritis due to bone growth and cartilage loss.The growth of bones in the last joints of the fingers is called the hibernate nodes.Bushar nodes are the growth of bones in the middle joints of the fingers.Knee joint cartilage can cause the outer curve of the knees (onion-feet).
- Shredded sound or grid sensation can be observed when arthritis moves.This is caused by bone bone or rough cartilage.
Usually, these symptoms do not arise suddenly and simultaneously, but gradually develop over time.Sometimes people do not recognize that they have osteoarthritis because they cannot remember for some time or injury that led to their symptoms.If the pain of the knee has worsened for several months, which does not respond to rest or change of activity, it is best to seek advice with a medical worker.
Diagnostics
Osteoarthritis can often be diagnosed with its characteristic symptoms of pain, reducing movement and/or deformation.Osteoarthritis can be confirmed by an X -ray or MRI scan.General data involves reducing the articular space between the bones, the loss of cartilage and bone backpacks, or the growth of bones.Blood tests can be used to exclude other possible conditions, but they cannot be diagnosed with osteoarthritis.

2 main processes are diagnosed in the OA knee OA.The first is based on a report on symptoms and clinical examination.A physiotherapist will ask questions about medical history and activities.The therapist will conduct a physical examination to measure the movement of the knee (movement range), strength, mobility and flexibility.They can also require various movements to see, increase or reduce pain.
The second tool used to diagnose the knee joint is a diagnostic visualization.A physiotherapist can send a physician who prescribes knee X-rays in different positions to inspect the knee joint bone and cartilage damage.
If the joints have a more serious injury to the suspect, you can order the MRI to more carefully study the overall status of articular and surrounding tissues.
Ordering blood tests can also help to exclude other conditions, which can lead to osteoarthritis -like symptoms of knee joints.
Treat
Depending on the severity of arthritis and the patient's age, it is selected how to treat knee joint arthrosis.Treatment may consist of operative or non -operative methods, or their combinations.
The first medicinal line of knee joint arthritis includes a modification of activity, anti -anti -aging and weight loss.Without action that exacerbates the pain, this condition can make it acceptable to some.Anti-inflammatory agents such as ibuprofen and COX-2 new inhibitors help alleviate inflammation, which can contribute to pain.
Physical therapy to strengthen the muscles around the knee will help to absorb the shock of the joint.This is especially true for arthritis with a knee-femoral knee bowl.Special types of bracelets designed for loading in the knee joint, which is less than arthritis, can also relieve pain.Injection of the drug inside the knee joint can also be temporarily helped.
In addition, the opposite side of the cane walking on the opposite side, as the painful knee can help distribute the load part, reduces pain.Lastly, weight loss helps reduce the force that passes through the knee joint.The combination of these non -operative measures can promote pain and disability caused by knee joint arthritis.
If inoperative methods do not allow you to make the condition tolerant, surgery may be the best option for the treatment of knee joint arthritis.The exact type of surgery depends on age, anatomy and the main condition.Some examples of surgical variants for the treatment of arthritis include osteotomy, which includes joint correction bone cutting and knee replacement surgery.
Modern methods of treating knee arthrosis include osteotomy, which is a good alternative if the patient is young and arthritis is limited to one area of the knee joint.This allows the surgeon to restore the knee to unload the arthritis area and carry the load on the relatively not involved knee.For example, the patient may restore the load on the joint.The advantage of this type of surgery is that the patient's knee joint is protected and may potentially provide many years of pain relief without the shortcomings of the prosthesis knee.Disadvantages include a longer rehabilitation course and the ability to develop arthritis of the recently leveled knee.
Knee joint replacement surgery involves cutting arthritis bone and adhering to the prosthesis joint.All arthritis surfaces have changed, including thigh, lower leg and knee bowl.Arthritis surfaces are removed, and the ends of the bone are replaced by prosthesis.The prosthesis component is usually made of metal and plastic surfaces designed for smooth sliding against each other.
The replacement of the knee joint
The overall knee joint replacement surgery was first performed in 1968 and has developed a reliable and effective way over the years to prevent pain when it is off and allows patients to resume their active life.Improvement in the field of surgical methods and implants has contributed to one of the most successful orthopedic procedures.The population becomes older and remains more active, the need for general knee replacement is still increasing.Many of the knee joint replacement operations were performed at a special surgery hospital.Improving surgical technology and designing new implants are a few contributions that surgeons have made.
People often wonder when and why they should change their knees.This is an individual question depending on the level of human activity and the level of functional needs.Many people with arthrosis live in pain, which impedes their participation in their activities;Others are so weak that it is difficult for them to wear shoes and socks.Complete replacement of the knee joint offers the problem of arthrosis and is carried out to relieve pain and resume activity.After rehabilitation after successful complete replacement of the knee joint, the patient may expect surgery without pain.Complete replacement of the knee joint significantly improves the patient's condition and significantly reduces long -term treatment costs.This study has shown that not only the overall replacement of the knee joint is economically effective not compared to surgical control, but also ensures greater functioning and the best quality of life.
Complete replacement of the knee joint is considered to be the main operation, and the solution is not trivial.Usually, people decide to undergo surgery when they think they can no longer live with arthritis.The implant consists of 4 parts: tibia, female parts, plastic tabs and patella.The components of the tibia and thigh are made of metal, usually with a cobalt chrome, used to lock the ends of the thigh and lower legs after removing the arthritis bone.The plastic tab is made of ultra -high molecular mass polyethylene and fits into the tibia component, so that the polished thigh surface slides along the plastic.The component of the knee bowl also grows on the front of the thigh component.Usually, they are attached to bone cement.
The complete replacement of the knee is performed in the operating room with a special laminar air flow system, which helps reduce the likelihood of infection.Your surgeon was wearing a "space space", which is also designed to reduce the likelihood of infection.The whole surgical team consists of your surgeon, from two to three assistants and a nanny.
Anesthesia is given by means of an epidural catheter, which is a small tube inserted in the back.This is the same type of anesthesia given to women in childbirth.During surgery, the patient can be both awakened and sleepy.
After the introduction of an epidural block around your thigh, a tourniquet or cuff will be placed.During surgery, the horizontal bar will be exceeded to reduce blood loss.Completely replacement of the knee is made along the front knee.The wound is measured from 4 to 10 inches, depending on the anatomy.
The surfaces of the thigh, lower legs and patella are subject to arthritis surfaces and are removed using strength tools.At the same time, the knee deformities are corrected and after surgery, the knee becomes more correct.The bone is ready to take an artificial knee joint and then apply a prosthesis.When closing, two drainage around the workplace is installed in the evacuation of blood.Sapers are used to close the skin.
The whole operation will take from 1 to 2 hours.After that, the patient will be taken to the recovery room where the tests will be checked.Most patients can be taken to ordinary room for several hours;Others should stay in the hall for recovery, as defined by a surgeon and anesthetic.

Patients usually stay in the hospital for 3-4 days after complete surgery.
Risks during surgery
Some risks of surgical procedure include blood loss, leg clotting, and the likelihood of infection.The general prevalence of these risks is very small.They should be discussed with the surgeon before surgery.
Some risks of prosthetic knee include the likelihood that parts are weakened or wear over time, or the prosthesis may be infected.Again, the surgeon is discussed on these issues.
Postoperative course
Upon complete operation of the knee joint, the patient will fall into the restoration room.Most patients can get into a regular ward after a few hours when the feeling returns to the legs.Given the pain pump that is connected to the epidural catheter, which will allow you to control when the pain is cured.Most people are quite comfortable with the help of a pain pump.
On the day of operation, you can perform some exercises as indicated by the physiotherapist, including the reduction of quadrants and moving the legs high and down.Depending on the advantages of surgery, you can start with the bent surgery of your new article or on the first day.The patient will be allowed to have the ice after surgery to bury the oral cavity, but drink fluid, or may cause nausea.The patient will have a catheter in the bladder, so you do not need to worry about urination.As soon as movement in the legs is restored, he will be allowed to sit, get up and take a few steps to the foot and the therapist.
The first day after surgery will be active, designed to support more mobile.Pacrant will meet with physiotherapists who instruct additional exercises.In addition, they will help you get up and walk in a few steps.Usually, the patient will be allowed to drink pure fluid.
It will be easier and easier to move in the coming days.The patient is released from pain and urine catheter.Pain treatment is taken as tablets.The next day after surgery, if there are signs of recovery in the intestines, it will be allowed to eat ordinary foods.
From your age, pre -operative physical condition and insurance cover, the patient may be a candidate for a short -term housing in the rehabilitation facility.Otherwise, the patient will be released home, and the physiotherapist will come home to continue the rehabilitation.The dispatcher discusses these options with the patient and helps him / her home.
Return to the activity surgeon and therapists will be guided.Patients can usually walk as much as they want 6 weeks after surgery.Patients can resume movement after 6 weeks.After 8 weeks, patients can refresh the game in golf and swim;Within 12 weeks they can play tennis.The surgeon will help decide what actions can be updated.
What is a physiotherapist
All physical therapists are made through education and clinical experience to treat various conditions or injuries:
- A physiotherapist who has experience in the treatment of people with osteoarthritis of the knee joint and changing the knee joint after surgery.Some physiotherapists have an orthopedic focus.
- A physiotherapist who is a certified orthopedic clinical specialist.This physiotherapist will have advanced knowledge, experience and skills that can be used for the state.
- You can find physiotherapists who have this and other accounting data using MRI, an online tool that will help you find physiotherapists with special clinical knowledge.
General Tip When You can find a physiotherapist (or other supplier of medical care):
- Get recommendations from family members and friends or other medical suppliers;
- To get involved in a physiotherapy clinic, you need to ask about the experience of physiotherapists in the help of people with arthritis.
At a first visit to the physiotherapist, you should be ready to describe the symptoms as much as possible and report the worsening symptoms.


































